The first study enrolled 111 consecutive patients, aged 51 to 95 years, presenting with invasive squamous cell carcinoma. The results are summarized in Table 3.25 Importantly, 30% of the tumors extended into the subcutaneous fat. The researchers recommend that excision of all squamous cell carcinomas should include subcutaneous fat (LOE: 2b).
The second study enrolled 117 patients with previously untreated, well-demarcated basal cell carcinoma. The investigators concluded that a 4-mm lateral margin will totally eradicate 98% of tumors <2 cm in diameter (3.79 mm; 95% confidence interval [CI], 3.21–4.86) (LOE: 2b).26 Vertical extension of tumor was not addressed. No recommendations were made for tumors 2 cm in diameter.
Interestingly, no tumors in this study required a 4-mm margin in all directions. Rather, the basal cell carcinomas were found to send out extensions in an irregular pattern.
TABLE 3
Surgical margins for treatment of squamous cell carcinomas 25
| Tumor diameter and risk level | Margin needed to completely clear 95% or more of tumors |
|---|---|
| 0–19 mm | 4 mm |
| ≥20 mm | 6 mm |
| “High-risk,”* 0–19 mm | 6 mm |
| “High-risk,”* 20 mm | Indeterminate† |
| *High risk of metastasis if located on scalp, ears, eyelids, nose, or lips (47 of 141 tumors in study located here). | |
| †Only 90% of tumors completely cleared even with 6 mm margin; author recommends Mohs surgery in this case. | |
Mohs micrographic surgery
Mohs surgery is generally considered the preferred treatment for high-risk primary non-melanoma skin cancer and recurrent non-melanoma skin cancer (LOE: 5).18 It is clearly superior for treatment of locally recurrent squamous cell carcinoma, with a 5-year cure rate of up to 90%, compared with 76.7% obtained with standard excision (LOE: 2a).27
The benefit of Mohs surgery for small (<1 cm), low-risk skin cancers is probably slight. Cure rates for primary nonmelanoma skin cancer are as high as 99.8% for basal cell carcinoma and 98.8% for squamous cell carcinoma, but standard excision also has high cure rates, up to 98% with proper surgical margins.19
Disadvantages include length of the procedure, need for special equipment, and dependence on highly trained personnel (a fellowshiptrained dermatologist and histotechnologist). Not surprisingly, availability of this procedure is limited. The high initial cost may be balanced by the lower cost of treating recurrent tumors, but no cost-effectiveness studies are available.28
Curettage and electrodesiccation
Curettage and electrodesiccation is performed using a sharp curette to remove soft material from the tumor until the underlying dermis is reached. The base of the tumor is then destroyed using hyfrecation. The procedure may be repeated once or twice to achieve a base of healthy tissue (LOE: 5).19,29
Curettage and electrodesiccation is the most common way dermatologists treat small (<1 cm) primary basal cell carcinoma.18 It is safe, well tolerated, and has 5-year cure rates >90%.5 Other advantages include speed and suitability for patients with multiple lesions.19 Curettage and electrodesiccation is also appropriate for small (<1 cm) primary squamous cell carcinoma below the neck (LOE: 5).22 This technique should not be used for malignant melanoma and is not suitable for tumors with high risk of metastasis or recurrence (LOE: 5).22
Cryosurgery
Cryosurgery with liquid nitrogen or nitrous oxide is used for small (<1 cm) superficial lesions and those locations where surgery is technically difficult, such as the lips, nose, ears, eyelids, and hands. It is also ideal for patients on chronic anticoagulation or with significant comorbidities.
For properly selected lesions, 5-year cure rates are excellent at 97% (LOE: 1a).20 Cure rates for larger lesions are reportedly high, but study follow-up was inconsistent (LOE: 2b).30 Small lesions heal completely in 4 to 6 weeks, while larger lesions may take up to 14 weeks to resolve (LOE: 5).31 Despite the prolonged healing time, cosmesis is often excellent.
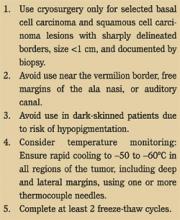
Guidelines for the treatment of non-melanoma skin cancer with cryosurgery are presented in Figure 5. Importantly, published cure rates for cryosurgery are based on several case series, the largest of which employed a temperature-monitoring thermocouple needle to guarantee adequate depth of freezing. Cryosurgery without a thermocouple device may therefore result in higher recurrence rates than expected.31
FIGURE 5
Guidelines for cryosurgery
Topical agents
Topical chemotherapeutic agents offer great promise in the treatment of properly selected tumors, but quality evidence is lacking. The most commonly used topical agent is the DNA synthesis inhibitor 5-fluorouracil (5-FU). 5-FU is a proven treatment for actinic keratoses and has been used to treat squamous cell carcinoma in situ and superficial basal cell carcinoma. However, 5-FU is contraindicated in invasive squamous cell carcinoma and basal cell carcinoma, as it may bury tumor tissue and lead to continued, subclinical spread (LOE: 5).19