CASE › For the third time in 9 months, 28-year-old Joan B comes into the office with complaints of painful, frequent, and urgent urination. Ms B is sexually active and her medical history is otherwise unremarkable. In each of the previous 2 episodes, her urine culture grew Escherichia coli, and she was treated with a 5-day course of nitrofurantoin. At this current visit, she asks about the need for additional work-up, treatment for her symptoms, and whether there is a way to prevent further infections.
Urinary tract infections (UTIs) are the most common bacterial infection in women1 and account for an estimated 5.4 million primary care office visits and 2.3 million emergency room visits annually.2 For women, the lifetime risk of developing a UTI is greater than 50%.3 In one study of UTI in a primary care setting, 36% of women under 55 and 53% of women over 55 had a recurrent infection within a year.4 Most women with UTI are treated as outpatients, but 16.7% require hospitalization.5 In the United States, direct costs for evaluation and treatment of UTI total $1.6 billion each year.5
Accurately characterizing recurrent UTI
Bacteriuria is defined as the presence of 105 colony forming units (ie, viable bacteria) per milliliter of urine collected midstream on 2 consecutive urinations.6 UTIs are symptomatic infections of the urinary tract and may involve the urethra, bladder, ureters, or kidneys.7 Infections of the lower tract (bladder and urethra) are commonly referred to as cystitis; infections of the upper tract (kidney and ureters) are referred to as pyelonephritis.
Most UTIs are uncomplicated and do not progress to more serious infections. However, patients who are pregnant, have chronic medical conditions (eg, renal insufficiency or use of immunosuppressant medications), urinary obstruction, or calculi may develop complicated UTIs.8
Recurrent UTI is an infection that follows resolution of bacteriuria and symptoms of a prior UTI, and the term applies when such an infection occurs within 6 months of the last UTI or when 3 or more UTIs occur within a year.7 Recurrent infection can be further characterized as relapse or reinfection. Relapse occurs when the patient has a second UTI caused by the same pathogen within 2 weeks of the original treatment.9 Reinfection is a UTI that occurs more than 2 weeks after completion of treatment for the original UTI. The pathogen in a reinfection may be the same one that caused the original UTI or it may be a different agent.9
It’s also important to differentiate between recurrent and resistant UTI. In resistant UTI, bacteriuria fails to resolve following 7 to 14 days of appropriate antibiotic treatment.9
Factors that increase the risk of recurrent UTI
Premenopausal women
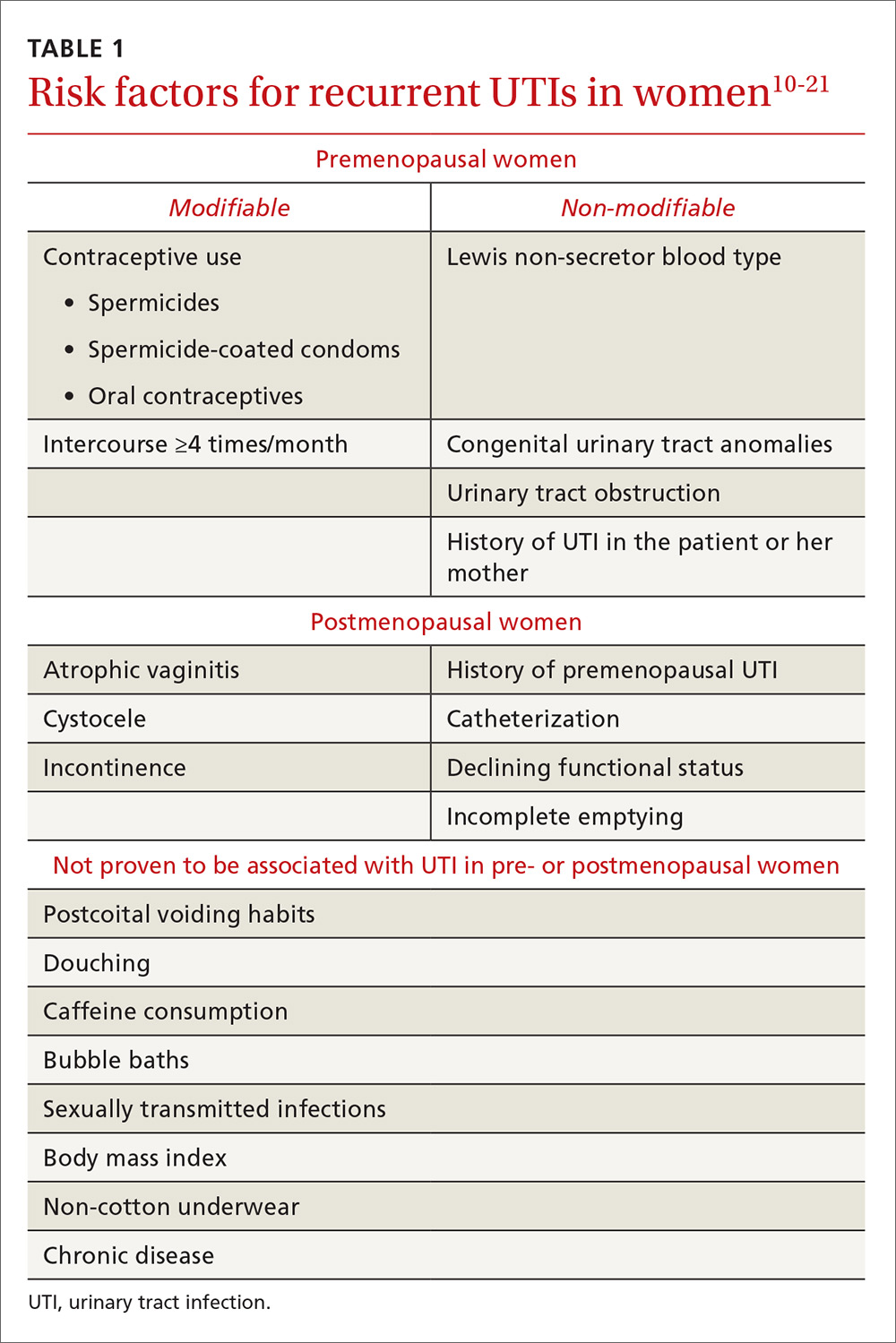
Both modifiable and non-modifiable factors (TABLE 110-21) have been associated with increased risk of recurrent UTI in premenopausal women. Among women with specific blood group phenotypes (Lewis non-secretor, in particular), rates of UTI rise secondary to increased adherence of bacteria to epithelial cells in the urinary tract.10 Other non-modifiable risk factors include congenital urinary tract anomalies, obstruction of the urinary tract, and a history of UTI.11,12 Women whose mothers had UTIs are at higher risk for recurrent UTI than are women whose mothers had no such history.13
Modifiable risk factors for recurrent UTI include contraceptive use (spermicides, spermicide-coated condoms, and oral contraceptives) and frequency of intercourse (≥4 times/month).13 Spermicides alter the normal vaginal flora and lead to increased colonization of E coli, which increases the risk for UTI.14 Women with recurrent UTIs were 1.27 to 1.45 times more likely to use oral contraceptives than those without recurrent UTIs.13 Compared with college women who had not had intercourse during the week, sexually active college women who had engaged in intercourse 3 times had a 2.6-fold increase in relative risk for UTI.15 Those who had daily intercourse had a 9-fold increase in relative risk of UTI development.15 This elevated risk is due to trauma to the lower urogenital tract (urethra) and introduction of bacteria into the urethra via mechanical factors.16,17
Postmenopausal women
Atrophic vaginitis, catheterization, declining functional status, cystocele, incomplete emptying, incontinence, and history of premenopausal UTIs are all risk factors for recurrent UTI in postmenopausal women.19,20 Decreased estrogen and resulting vaginal atrophy appear to be associated with increased rates of UTI in these women. Additionally, postmenopausal women’s vaginas are more likely to be colonized with E coli and have fewer lactobacilli than those of premenopausal women,21 which is thought to predispose them to UTI. These risk factors are summarized in TABLE 1.10-21
Initial evaluation of recurrent UTI
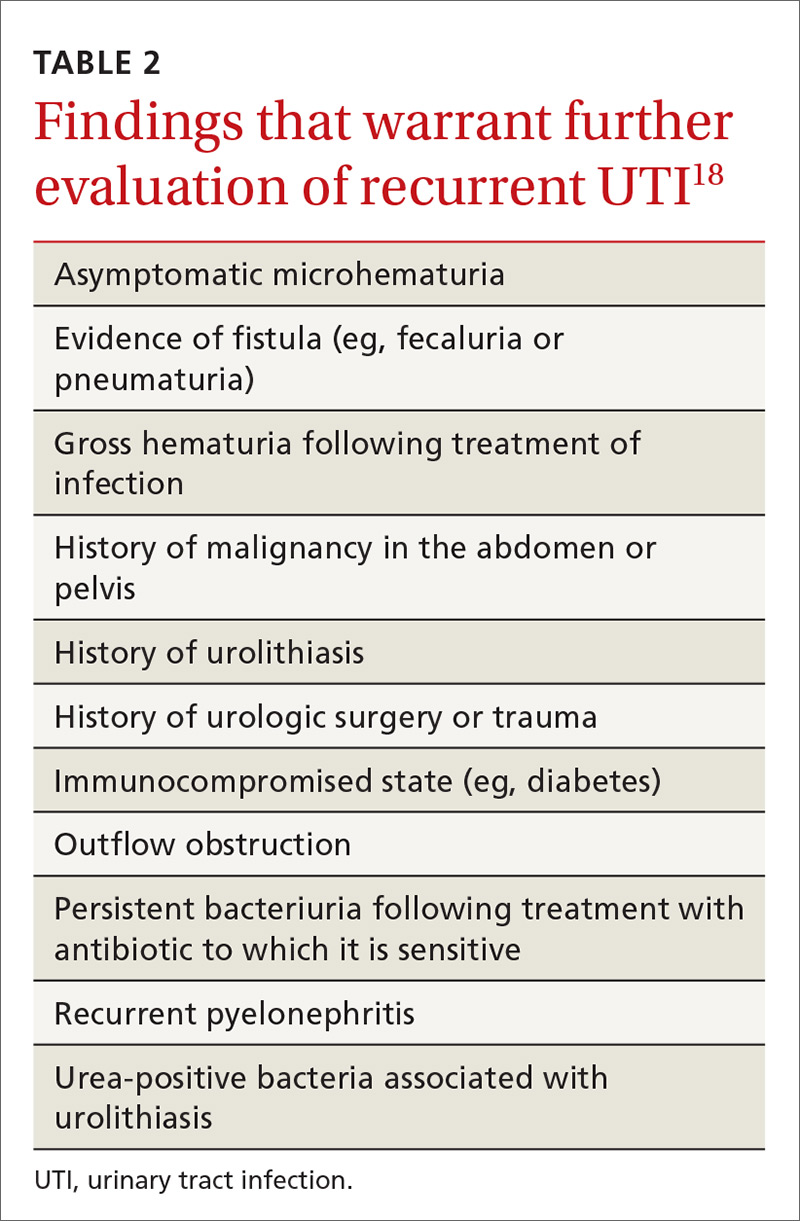
Patients with recurrent UTI experience signs and symptoms similar to those with isolated uncomplicated UTI: dysuria, frequency, urgency, and hematuria. Focus your history interview on potential causes of complicated UTI (TABLE 218). Likewise, perform a pelvic examination to evaluate for predisposing anatomic abnormalities.22 Finally, obtain a urine culture with antibiotic sensitivities to ensure that previous treatment was appropriate and to rule out microbes associated with infected uroliths.18 Given the low probability of finding abnormalities on cystoscopy or imaging, neither one is routinely recommended for the evaluation of recurrent UTI.18