Monoamine oxidase inhibitors (MAOIs) have well-established efficacy for treating depression, panic disorder, and social phobia. However, a lack of familiarity with these agents and misconceptions about the risks associated with their use have led to MAOIs being substantially underutilized. The goal of this 2-part guide to MAOIs is to educate clinicians about this often-overlooked class of medications. Part 1 (“A concise guide to monoamine inhibitors,” Current Psychiatry. December 2017, p. 14-23,47,A) described the pharmacology of MAOIs, the mechanism by which tyramine induces hypertension in patients taking MAOIs, and what to tell patients about dietary restrictions associated with these medications. Part 2 covers how to avoid potential drug interactions, including serotonin syndrome (SS) and pressor effects, that could affect patients receiving an MAOI; other factors to consider when starting a patient on an MAOI; and augmentation strategies for depressed patients who do not achieve remission from MAOI monotherapy.
MAOIs and potential drug interactions
One source of concern in patients receiving irreversible nonselective MAOIs is the development of excessive serotonergic neurotransmission resulting in SS. In the 1960s, researchers noted that administering large doses of tryptophan to MAOI-treated patients resulted in clonus and hyperactive reflexes without hypertensive events.1 In 1991, Sternbach2 provided an extensive case series and described the first set of criteria for SS. Features of SS include:
- mild symptoms: tremor, akathisia, inducible clonus
- moderate symptoms: spontaneous or sustained clonus, muscular hypertonicity
- severe symptoms: hyperthermia, diaphoresis.2
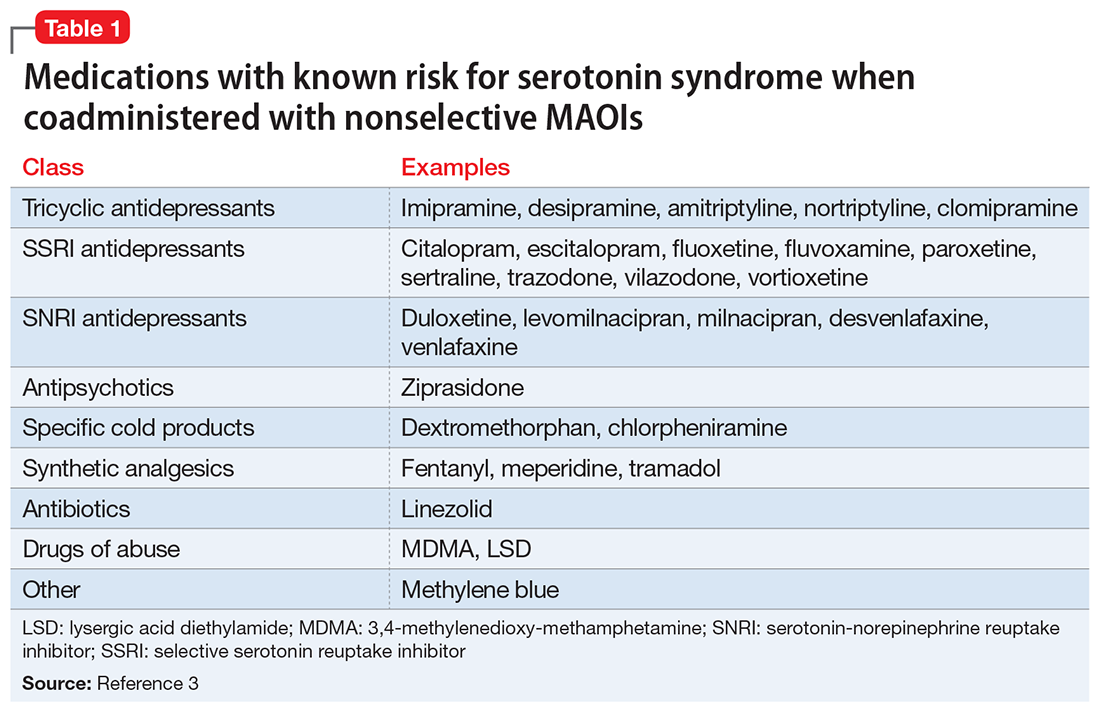
Although SS can be induced by significant exposure to individual agents that promote excess synaptic serotonin (eg, overdose of selective serotonin reuptake inhibitors [SSRIs]), the majority of fatal cases have occurred among patients taking MAOIs who were coadministered an agent that inhibited serotonin reuptake (Table 13). Animal studies have determined that excessive stimulation of the 5HT2A receptor is primarily responsible for SS,4 and that 5HT2A antagonists, such as mirtazapine, can block the development of SS in a mouse coadministered fluoxetine and tranylcypromine.5 In addition to a patient’s medication history, the clinical hallmark of SS that helps distinguish it from neuroleptic malignant syndrome, delirium, and other acute syndromes is clonus, which becomes spontaneous and sustained as the severity increases.
Risk for SS. Most medications that promote serotonergic activity are well known for their use as antidepressants, but other agents that have 5HT reuptake properties (eg, the antihistamine chlorpheniramine) must be avoided. Although older literature suggests that the use of lower doses of certain tricyclic antidepressants concurrently with MAOIs may not be as dangerous as once believed,6 there are sufficient reports of serious outcomes that tricyclics should be avoided in patients taking MAOIs because of the risk of SS, and also because, in general, tricyclics are poorly tolerated.7