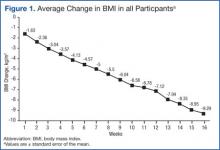
BMI decreased linearly during the intervention (Figure 1). In 10 subjects, the change in BMI postintervention was both statistically (-16 ± 8%, P < .0001) and clinically significant and sufficient for surgical clearance. Eight (40%) had surgery and 2 (10%) no longer needed surgery due to self-reported improved quality of life and decreased pain. Despite the clinically and statistically significant weight loss, 14.5% of the weight lost was fat-free mass; decrease in body fat was 9% ± 4% (P < .0001).
All study subjects consumed 5 Optifast packets per day for at least 10 weeks and no longer than 16 weeks. Of the participants who completed the intervention, the majority elected to continue the intervention time to 16 weeks; however 1 participant went to week 10 and 2 participants completed through week 13. Nonadherence in this protocol was defined as > 2 weeks of weight gain. Two participants gained weight for 6 and 7 weeks, respectively.
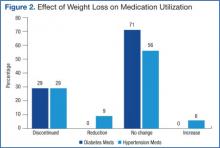
Mean systolic blood pressure, plasma triglyceride and fasting glucose levels, A1c, and REE levels decreased significantly postintervention. Additionally, patients experienced either dose reduction or discontinuation of diabetes or hypertension medication use postintervention (Figure 2). Discontinued diabetes medications included rosiglitazone (n = 1), glyburide (n = 1), and metformin (n = 2). Discontinued or reduced antihypertensives included furosemide (n = 1), thiazides (n = 3), beta blockers (n = 1), angiotensin-converting enzyme inhibitors (n = 4), calcium channel blockers (n = 2), and angiotensin II receptor antagonists (n = 2).
Discussion
To the authors’ knowledge, this was the first study using a low calorie liquid diet to achieve weight loss to qualify for nonbariatric elective surgery. This diet provides an alternative intervention for individuals who would otherwise be denied elective surgery due to extreme obesity. Eighty percent of participants completed 10 to 16 weeks of the 800 calorie liquid diet plan with significant weight loss of 16 BMI ± 8%. The intervention was well tolerated without significant AEs.
It is difficult to compare these results to prior studies, as the target populations differ. Previous studies utilizing calorie levels < 800 calories per day included mostly women and consequently, their preintervention weights were lower than in the current study population.10 This study population was predominately older males with a high prevalence of comorbid medical and psychiatric conditions. Despite these demographic and clinical differences, improvements in biochemistries were similar to those demonstrated previously.8-10 The observations for beneficial changes in cardiovascular and glycemic risk factors and reduced medication use related to weight loss and calorie control are consistent with previous results.8-10
Related: Moral Questions Surrounding Bariatric Surgery
To the authors’ knowledge, REE has not been reported in earlier investigations of very low calorie diet interventions. This study found significant decreases in REE, which was measured pre- and postintervention. Participants were given postintervention REE value and individualized meal plans were developed from this number. An interesting and unexpected finding was that this number seemed to provide useful reinforcement for patients as they transitioned to solid food. This may have helped improve adherence to meal plans. Despite concerns regarding possible weight gain, the weight loss continued at a similar rate during the transition, demonstrating that continued weight loss can occur with a combination of food and liquid diet.
The need for elective surgery may have increased motivation to adhere to this weight-loss program. The dropout rate was 20%; lower than previous studies using very low calorie diets and substantially better than traditional weight-loss programs.8,9
An unexpected finding was that 10% of participants who qualified for knee replacement surgery chose to postpone surgery due to decreased pain and improved quality of life. Over the past 20 years, the estimated cost of 1 TKA was $15,000 with an estimated $9 billion spent annually for this procedure in the U.S.26 Importantly, obesity increases the risk of TKA revision surgeries, which are both expensive (average cost of Medicare-covered TKA revision surgeries is $73,696) and projected to increase 66% over the next 25 years.27 Weight loss prior to surgery not only may decrease risk for revisions of TKA, but in some cases also may delay or eliminate the need for surgery.
Although there are significant costs associated with certain weight loss programs, the savings associated with reducing the need for surgery would be substantially greater than that associated with the dietary intervention. The estimated private sector cost of an 18-week weight-loss program (12-week liquid with 6-week transition) is $3,500 per participant. This study program was estimated to cost $2,400 per participant for the 16-week (13-week liquid diet and 3-week transition) program. Patients with obesity awaiting orthopedic, gastrointestinal, or neurosurgery were often referred for bariatric surgery to obtain weight loss. Bariatric surgery averages $17,000 to $26,000, which is more expensive than this diet program.28