SNOWMASS, COLO. – For all the talk of embracing the heart team approach to coronary revascularization as the new standard, emphasizing interdisciplinary collaboration between cardiologists and surgeons, hybrid coronary revascularization remains a rarely employed strategy.
Hybrid coronary revascularization (HCR) is performed at one-third of U.S. centers providing coronary artery bypass graft (CABG) surgery, but that’s a misleading statistic. A mere handful of the centers have extensive experience with this strategy, according to the first nationwide assessment of HCR in patients with multivessel coronary artery disease.
“Only a very few centers – maybe 5 or 10 – do hybrid procedures as 8%-10% of their volume,” Dr. Vinod H. Thourani* said at the Annual Cardiovascular Conference at Snowmass.
He was a coinvestigator in the analysis of nearly 200,000 CABG procedures in the Society of Thoracic Surgeons (STS) national database for 2011-2013. Hybrid coronary revascularization – a combination of surgical and percutaneous techniques coupling minimally invasive bypass of the left anterior descending (LAD) coronary artery using an internal mammary artery graft along with drug-eluting stents for non-LAD lesions – accounted for just 0.48% of total CABG volume. And no trend for growth in the HCR approach was evident during the study period.
Moreover, even in the one-third of U.S. CABG centers that performed hybrid coronary revascularization, the strategy was used on average in less than 1% of all CABG procedures (Circulation 2014;130:872-9), noted Dr. Thourani, professor of cardiothoracic surgery and codirector of the Structural Heart and Valve Center at Emory University, Atlanta.
In contrast, he and his Emory colleagues have fully embraced HCR. At Emory, even as the annual number of primary isolated CABG procedures with sternotomy fell by 44% from 2005 to 2012, there was a compensatory increase in the number of HCRs.
“We’ve actually maintained our coronary bypass volume based on introducing HCR, unlike a lot of programs,” according to the surgeon.
The appeal of HCR is that it combines the durability of the internal mammary artery-to-LAD graft – long recognized as the main source of the survival advantage CABG holds over percutaneous interventions – with drug-eluting stents as a less invasive alternative to often-unreliable vein grafts in non-LAD target vessels.
The current American College of Cardiology/American Heart Association guidelines on coronary revascularization give HCR a favorable class IIa recommendation. However, since there are few data on clinical outcomes with HCR versus conventional CABG, Dr. Thourani and his coinvestigators compared in-hospital outcomes in the STS database. They found that after adjustment for the higher cardiovascular risk profiles present in patients undergoing HCR, the rates of in-hospital mortality and major morbidity in the two groups were similar, suggesting HCR may offer an equally safe alternative to CABG in selected patients.
Patients want less invasive alternatives to CABG with sternotomy. The three most common minimally invasive, sternal-sparing approaches are minimally invasive direct coronary artery bypass, or MIDCAB; robotic-assisted totally endoscopic coronary artery bypass, or TECAB; and robotic-assisted coronary artery bypass, a favored approach at Emory. In robotic-assisted coronary artery bypass, the harvest of the left internal mammary artery, pericardiotomy, and targeting of the LAD are accomplished with robotic assistance, but the anastomosis is hand sewn under direct vision, off pump, via a non–rib-spreading 3- to 4-cm minithoracotomy.
In a report on 307 consecutive patients who underwent robotic-assisted CABG at the university, including 159 who had HCR for multivessel disease, short-term clinical and angiographic outcomes were excellent (J. Thorac. Cardiovasc. Surg. 2014;147:179-85). Particularly striking, in Dr. Thourani’s view, was that only one postoperative stroke occurred, for a 0.3% incidence. That’s a far lower rate than typical with CABG with vein grafts.
In a more recent, as-yet-unpublished update including 477 consecutive HCR patients at Emory, the stroke rate remained extraordinarily low at 0.2%, he said.
“You can almost eliminate stroke with this procedure,” according to Dr. Thourani.
Thirty-day mortality was 0.8%, with an MI rate of 1.0%, a 3.8% incidence of conversion to sternotomy, and a 1.9% repeat revascularization rate. The rate of Fitzgibbon A patency was 96.2%, he noted.
“Return to work is really at the patient’s discretion. We tell them, ‘when you don’t hurt, you can go back.’ Some people go back 4-5 days after surgery. And there are really zero limitations for the patient – none whatsoever,” the surgeon said.
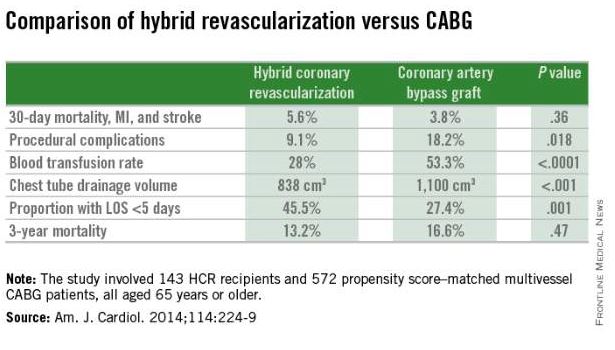
The HCR approach to multivessel revascularization appears to be particularly advantageous in diabetic patients and in older individuals. In a retrospective, nonrandomized single-center comparison of 143 HCR recipients who were propensity score matched to 572 patients who underwent multivessel CABG (Am. J. Cardiol. 2014;114:224-9), the HCR recipients had significantly fewer procedural complications, faster recovery, and similar 3-year mortality (see graphic).