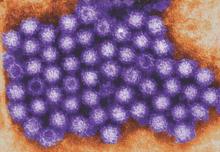
The global economic impact of norovirus is roughly $60 billion in societal costs and $4 billion in direct health care costs per year, according to an simulation model analysis.
Most of the costs (84%-99%, varying by region) resulted from lost productivity. The total societal cost was highest in children younger than 5 years, nearly $40 billion, compared with $20 billion for all other age groups combined, but the cost per illness was highest among adults aged 55 years and older.
Disease incidence was similar across all countries in the simulation model that included 233 countries stratified by World Health Organization region and globally but high-income countries accounted for 62% of the global health system costs, wrote Sarah M. Bartsch of Johns Hopkins University, Baltimore, and colleagues (PLoS ONE 2016. doi: 10.1371/journal.pone.0151219).
In the United States, norovirus was the most common pathogen identified in cases of acute gastroenteritis (AGE, 6%), followed by rotavirus and sapovirus (2% for both) and astrovirus (1%), according to data from a population-based study, including 1,099 stool specimens collected between August 2012 and September 2013. These findings were published in a separate study (PLoS ONE 2016. doi: 10.1371/journal.pone.0148395).
Overall, U.S. children younger than 5 years of age had the highest prevalence of norovirus; outpatient incidence and community incidences were 25.6 and 152.2 per 1,000 person-years, respectively. The next highest norovirus prevalence occurred in adults older than 65 years; outpatient and community incidence were 7.8 and 7.8 per 1,000 person-years, respectively. The study provides “the first U.S. laboratory-based age-specific norovirus AGE incidence rates in both community and outpatient settings,” wrote Scott P. Grytdal of the Centers for Disease Control and Prevention in Atlanta, and colleagues.