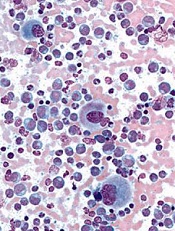
Credit: UC San Diego
Preclinical research in chronic myeloid leukemia (CML) has pointed to a relationship between cell adherence and treatment resistance.
Investigators found that a population of plastic-adherent K562 cells with increased expression of BCR-ABL exhibited greater resistance to the tyrosine kinase inhibitor imatinib than nonadherent K562 cells.
“Previous studies have linked high levels of the BCR-ABL mutation with drug resistance,” said Richard Byers, PhD, of The University of Manchester in the UK.
“We wanted to see how expression of BCR-ABL differed across groups of CML cells and, in particular, whether there were differences between adherent and nonadherent populations.”
Dr Byers and his colleagues described this investigation in Experimental Hematology.
The researchers evaluated the heterogeneity of BCR-ABL expression at DNA, messenger RNA, and protein levels, using the CML-derived K562 cell line.
They grew cells in suspension and found that some cells adhered to the plastic dish. The investigators then separated the plastic-adherent and nonadherent cell populations and studied them as single cells and in bulk.
The first discovery was that adherent and nonadherent cells had similar BCR-ABL fusion gene copy numbers.
In bulk-cell analysis, the mean relative normalized ratio for genomic ABL DNA copy number was 47.73 for adherent cells and 53.40 for nonadherent cells (P=0.11). In single-cell analysis, the mean copy numbers were 13.83 and 14.22, respectively (P=0.63).
On the other hand, there was a significant difference in BCR-ABL messenger RNA expression between adherent and nonadherent cells.
In bulk cells, the level of BCR-ABL messenger RNA transcripts was 11-fold higher in adherent cells than in nondherent cells (P=0.022). And single-cell analysis revealed the mean BCR-ABL copy number was 53.11 for adherent cells and 14.06 for nonadherent cells (P=0.0013).
Adherent cells also exhibited significantly upregulated phosphorylation of BCR protein compared to nonadherent cells.
Flow cytometry showed that a mean of 61.9% of adherent cells were positive for phosphor-BCR, compared to 14.5% of nonadherent cells (P=0.0074). And single-cell analysis revealed a mean signal number per cell of 8.23 among adherent cells and 3.02 among nonadherent cells (P<0.0001).
In addition, whole-genome microRNA profiling showed that adherent and nonadherent cell populations expressed significantly different microRNA species.
Finally, the researchers found that treatment with imatinib reduced cell viability more rapidly in nonadherent cells than in adherent cells (P<0.005). The adherent cells showed a decrease in cell viability at 24 hours, compared to 4 hours for nonadherent cells.
The investigators said this research suggests that CML patients may have a similar adherent cell population that mediates resistance to imatinib. And the study highlights the importance of single-cell analysis.
“The small number of cells that show high levels of BCR-ABL may not be detectable through bulk analysis of large samples,” Dr Byers said. “It looks like it is important to look at protein levels in single cells.”
“In future, it may be possible to measure BCR-ABL levels in individual cells in the clinic. This will help us identify the resistant, high-BCR-ABL cells and better understand how patients develop resistance to imatinib treatment, with the aim of combating this resistance to make response more durable and the treatment more effective.”

