CE/CME
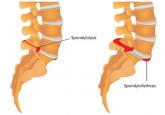
Spondylolysis and Spondylolisthesis Primary Care Clinicians' Role
Although accreditation for this CE/CME activity has expired, and the posttest is no longer available, you can still read the full article....
Deedra Harrington, DNP, MSN, APRN, ACNP-BC, Janis R. Guilbeau, DNP, RN, FNP-BC, Christy McDonald Lenahan, DNP, MSN, APRN, FNP-BC
A-FIB CLASSIFICATION
For purposes of choosing appropriate therapy, it is necessary to determine whether the cause of A-fib is valvular or nonvalvular. Valvular A-fib is described as A-fib that occurs in the presence of valvular heart disease or defect, such as rheumatic mitral stenosis, a mechanical or bioprosthetic heart valve, or mitral valve repair.1 In the absence of these types of conditions, A-fib is considered nonvalvular. The vast majority of patients have nonvalvular A-fib; in the ATRIA (AnTicoagulation and Risk Factors In Atrial Fibrillation) study, researchers found that, among 17,974 adults with A-fib who were members of a large California health maintenance organization, only 4.9% had valvular heart disease.8
A-fib is commonly classified into four subcategories, based on its duration: paroxysmal, persistent, longstanding persistent, and permanent.
Paroxysmal. The occurrence of at least two episodes that have terminated in less than seven days without treatment.
Persistent. An episode lasting more than seven days or less than seven days after electric or pharmacologic conversion.
Longstanding persistent. Continuous A-fib for more than one year.
Permanent. A category for patients in whom rhythm control is no longer being pursued.
This simplified classification is often used to choose between ablative or medication therapies. To ensure accuracy, however, underlying causes, risk factors, and mechanisms should be determined.9
Stroke risk calculation
Once nonvalvular A-fib is confirmed, the next step is to control the ventricular rate and attempt to convert the A-fib rhythm. To accomplish this, the patient’s risk for stroke must be estimated and the need for oral anticoagulation determined.
The CHADS2 risk stratification system for calculating an individual’s risk for ischemic stroke in A-fib was developed in 2001. The risk criteria used in the calculation are Congestive heart failure, Hypertension, Age ≥ 75 years, Diabetes mellitus, prior Stroke, transient ischemic attack, or thromboembolism.10
Recent additions to the criteria account for advanced age, gender, and known vascular disease.1,5 Known as the CHA2DS2-VASc, this scoring system is outlined in Table 2. If the patient’s score is 0, risk for stroke is low and anticoagulation therapy is not recommended. If the score is 1, the risk is intermediate, and the patient may be treated with aspirin therapy or anticoagulation. With a CHA2DS2-VASc score of 2 or greater, anticoagulation treatment is recommended to reduce the risk for stroke.1
While the expanded CHA2DS2-VASc criteria more clearly define the basis for an anticoagulation recommendation—particularly in older patients, women, and those with a vascular history—the superiority of one over the other is undetermined.11 However, the 2014 American Heart Association/American College of Cardiology/Heart Rhythm Society (AHA/ACC/HRS) guidelines for the management of patients with A-fib recommend use of the CHA2DS2-VASc.1
Continue for anticoagulation therapy >>
Although accreditation for this CE/CME activity has expired, and the posttest is no longer available, you can still read the full article....
Although accreditation for this CE/CME activity has expired, and the posttest is no longer available, you can still read the full article.

Although accreditation for this CE/CME activity has expired, and the posttest is no longer available, you can still read the full article....
